What Is PCOS?
PCOS affects 8-13% of reproductive-age women worldwide and is characterized by elevated male hormones (androgens), irregular periods, and often small cysts on the ovaries.
Unlike the natural hormonal transition of menopause, PCOS typically begins during reproductive years and continues throughout a woman's lifetime.
Key characteristics of PCOS include:
- Elevated testosterone and other androgens
- Insulin resistance in 50-70% of cases
- Irregular or absent menstrual cycles
- Potential fertility challenges
- Symptoms like acne, excess hair growth, and scalp hair loss
What Is Andropause?
Andropause, sometimes called "male menopause," is the gradual decline of testosterone in men, typically beginning around age 40-50.
Unlike menopause in women, which occurs over a relatively short timeframe, andropause progresses slowly over decades with testosterone decreasing approximately 1-2% per year.
Common features of andropause include:
- Gradually decreasing testosterone levels
- Increased body fat, particularly around the abdomen
- Decreased muscle mass and strength
- Reduced energy levels and changes in mood
- Decreased libido and potential erectile dysfunction
PCOS vs Andropause: Comparing Female and Male Hormonal Changes
Hormone Direction: Excess vs. Decline
The most significant contrast between PCOS and andropause is the direction of hormonal change. Women with PCOS experience androgen excess—elevated levels of "male" hormones like testosterone—while men in andropause face androgen decline with decreasing testosterone production.
These opposite hormone trajectories create distinctly different symptom profiles and health concerns, even though both conditions involve the same hormones.
Age of Onset and Duration
PCOS typically begins around puberty or early adulthood and continues throughout a woman's reproductive years and beyond. Andropause, by contrast, is part of the natural aging process in men, typically beginning in the 40s or 50s.
While PCOS is a lifelong condition requiring ongoing management, andropause is a gradual transition that eventually stabilizes, albeit at lower testosterone levels.
Insulin Resistance Connection
Both conditions share a relationship with insulin resistance, but the connection is stronger and more central in PCOS. For many women with PCOS, insulin resistance is a driving factor behind elevated androgens.
In andropause, insulin resistance may develop as a consequence of decreased testosterone rather than as a primary cause.
This difference explains why insulin-sensitizing medications like metformin or inositol are often beneficial for PCOS but less commonly prescribed for andropause.
Body Composition Changes
Both conditions affect body composition, but in different ways:
- PCOS: Higher androgens can contribute to central (abdominal) fat distribution, despite women naturally having higher body fat percentages than men
- Andropause: Lower testosterone leads to decreased muscle mass and increased body fat, often around the abdomen
Interestingly, the body composition changes in both conditions tend to increase cardiovascular risk factors, though through different hormonal mechanisms.
Emotional and Psychological Impacts
Both PCOS and andropause can affect mood and mental health, but women with PCOS face unique challenges related to body image, fertility concerns, and the visible symptoms of hyperandrogenism like acne and hirsutism.
Women with PCOS are more likely to experience depression and anxiety compared to women without the condition.
Men experiencing andropause may notice mood changes, irritability, and decreased motivation, but these symptoms typically evolve gradually and without the same stigma that often accompanies visible PCOS symptoms.
Managing Hormonal Changes: Practical Strategies
Diet and Nutrition Approaches
While both conditions benefit from healthy eating, the specific dietary recommendations differ slightly:
- For PCOS: Focus on blood sugar management with lower glycemic load foods, adequate protein, and anti-inflammatory choices like those found in a Mediterranean-style eating pattern. Consider trying liver-supporting foods and collagen-rich options.
- For Andropause: Emphasize protein intake to support muscle maintenance, along with healthy fats that support hormone production.
Both conditions benefit from limiting processed foods, added sugars, and inflammatory fats found in highly processed vegetable oils like canola oil (compared to healthier options like avocado oil).
Exercise Considerations
Physical activity benefits both conditions but with different emphasis:
- For PCOS: Both strength training and moderate-intensity cardio can improve insulin sensitivity. High-intensity interval training (HIIT) may be particularly beneficial but should be balanced with recovery.
- For Andropause: Resistance training becomes increasingly important to maintain muscle mass and bone density as testosterone declines.
For both conditions, consistency matters more than intensity, and finding enjoyable activities increases long-term adherence.
Supplement Considerations
Some supplements that may benefit women with PCOS include inositol, vitamin D, zinc, and magnesium. Men experiencing andropause might consider vitamin D, zinc, and magnesium as well.
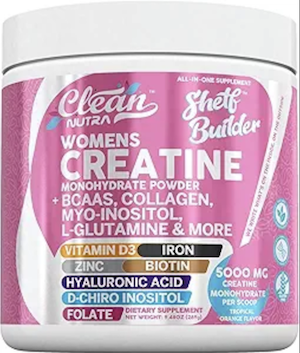 Interestingly, creatine supplementation may benefit both conditions—supporting strength training benefits for women with PCOS while helping maintain muscle mass for men experiencing andropause.
Interestingly, creatine supplementation may benefit both conditions—supporting strength training benefits for women with PCOS while helping maintain muscle mass for men experiencing andropause.
Always consult with healthcare providers before starting any supplements, as individual needs vary significantly.
When to Seek Medical Support
For women with PCOS, working with healthcare providers familiar with the condition is essential for proper diagnosis and management. Reproductive endocrinologists, gynecologists with PCOS expertise, and integrative practitioners can offer valuable support.
Men experiencing significant andropause symptoms may benefit from consulting with urologists, endocrinologists, or physicians specializing in men's health or anti-aging medicine.
Both conditions benefit from a team approach that may include nutritionists, mental health professionals, and fitness specialists alongside medical care.
Frequently Asked Questions
Does PCOS ever go away like andropause eventually stabilizes?
Unlike andropause, which eventually stabilizes at lower testosterone levels, PCOS is a lifelong condition. However, symptoms can change significantly throughout a woman's life, particularly after menopause when ovarian hormone production naturally declines.
Many women find their PCOS symptoms improve with age, though insulin resistance and cardiovascular risks may persist. Many women find certain PCOS challenges improve after menopause, though metabolic concerns may persist.
Learn more: https://app.pcosmealplanner.com/knowledge-articles/any/pcos-vs-andropause-female-vs-male-hormonal-changes">Tweet this
Can women experience something similar to andropause when they go through menopause?
Yes, women experience menopause—the cessation of menstrual cycles due to declining estrogen and progesterone. However, women with PCOS may experience menopause differently than women without PCOS. Some research suggests women with PCOS may reach menopause about two years later on average.
After menopause, androgens still tend to be higher in women who had PCOS, though the difference becomes less pronounced. Learn more about PCOS across the lifespan: https://app.pcosmealplanner.com/knowledge-articles/any/pcos-vs-andropause-female-vs-male-hormonal-changes">Tweet this
Do testosterone treatments for men with andropause cause similar symptoms to PCOS?
While testosterone replacement therapy (TRT) for men with andropause aims to restore testosterone to normal physiological levels, excessive testosterone supplementation can cause side effects like acne, mood changes, and cardiovascular concerns.
However, these effects differ from PCOS because the underlying hormonal environment and genetic factors are different.
Women with PCOS have female reproductive systems responding to inappropriate levels of androgens, while men receiving TRT have male reproductive systems being supplemented with hormones their bodies naturally produce.
Learn about comparing male and female hormone changes: https://app.pcosmealplanner.com/knowledge-articles/any/pcos-vs-andropause-female-vs-male-hormonal-changes">Tweet this
Can diet changes that help PCOS also benefit men with andropause?
Yes, there is significant overlap in helpful dietary approaches. Both conditions benefit from anti-inflammatory eating patterns that support insulin sensitivity, like Mediterranean-style diets rich in vegetables, quality proteins, healthy fats, and limited processed foods.
However, specific macronutrient balances may differ—men with andropause often benefit from slightly higher protein intake to preserve muscle mass, while women with PCOS may need more careful carbohydrate selection to manage insulin response. Tweet this
Is excess facial hair in PCOS similar to male pattern facial hair?
The hirsutism (excess facial and body hair) that many women with PCOS experience follows male-pattern distribution but typically doesn't reach the density or coarseness of male facial hair unless androgen levels are extremely high.
This is because women with PCOS still have female genetic makeup and baseline hormonal environments, with relatively elevated but not male-equivalent androgen levels.
Treatment approaches for hirsutism include addressing underlying hormonal imbalances through lifestyle and medications, along with hair removal methods.
Both medical and cosmetic approaches can help manage this challenging symptom. https://app.pcosmealplanner.com/knowledge-articles/any/pcos-vs-andropause-female-vs-male-hormonal-changes">Tweet this
Understanding the differences and similarities between PCOS and andropause highlights how the same hormones—in excess or deficiency—create entirely different health challenges across biological sexes.
For women managing PCOS, this knowledge can provide perspective on your hormonal health journey and help you make informed decisions about treatment approaches.
Remember that both conditions are increasingly well-understood and treatable with appropriate medical care and lifestyle strategies.
With personalized support, both women with PCOS and men experiencing andropause can maintain quality of life and minimize health risks associated with their hormonal changes.

Community Comments
Community Comments
Add a comment