Getting a pcos diagnosis in the UK can feel overwhelming, especially when symptoms have been dismissed or misunderstood. Understanding the process, criteria, and your rights within the NHS system empowers you to advocate for proper care and timely diagnosis.
With PCOS affecting up to 1 in 10 women in the UK, yet over 60% experiencing difficulties receiving diagnosis, knowing how to navigate the system is crucial for getting the help you need.
Understanding PCOS Diagnosis Criteria in the UK
The NHS uses the internationally recognized pcos diagnosis criteria known as the Rotterdam criteria. A diagnosis of PCOS can usually be made if other causes have been ruled out and you meet at least 2 of these 3 criteria:
- Irregular or infrequent periods - indicating your ovaries don't regularly release eggs (ovulation issues)
- High levels of male hormones - shown through blood tests or physical signs like excess hair growth, acne, or male-pattern hair loss
- Polycystic ovaries - visible on ultrasound scan showing multiple small follicles
Importantly, you don't need all three symptoms for a diagnosis of pcos. This "2 out of 3" approach means many women who previously went undiagnosed can now receive proper care and treatment.
Important Note: The NHS emphasizes that you don't necessarily need an ultrasound scan before PCOS can be confirmed if the other two criteria are clearly met.
Step-by-Step Guide: How to Get a PCOS Diagnosis
Step 1: Book a GP Appointment
Start with your GP, who can initiate the pcos diagnosis test process. Prepare for your appointment by:
- Tracking your menstrual cycle for 2-3 months (noting dates, flow, and symptoms)
- Documenting PCOS symptoms like weight gain, hair growth patterns, acne, or mood changes
- Listing family history of PCOS, diabetes, or hormone-related conditions
- Bringing any previous test results or medical records
Step 2: Initial Assessment and History
Your GP will take a comprehensive medical history, including:
- Menstrual and fertility history
- Weight changes and eating patterns
- Current medications and contraceptive use
- Family medical history
- Blood pressure check
Key Tip: If you're taking hormonal contraception, discuss stopping it 3 months before testing, as it can mask PCOS symptoms and affect hormone level accuracy.
Step 3: Blood Tests for PCOS Diagnosis
Essential blood tests for pcos diagnosis typically include:
- Hormone panel: Testosterone, LH (luteinising hormone), FSH (follicle-stimulating hormone), and SHBG (sex hormone-binding globulin)
- Thyroid function: TSH and T4 to rule out thyroid disorders
- Prolactin levels: To exclude hyperprolactinemia
- Glucose and insulin: Fasting glucose, HbA1c, and sometimes insulin levels
- Lipid profile: Cholesterol and triglycerides
Some areas may also test for androstenedione, which NHS guidelines note as "a more sensitive indicator of PCOS than calculation of FAI (Free Androgen Index)."
Step 4: Ultrasound Scan (If Required)
A pcos diagnosis ultrasound may be arranged if:
- You have clinical features of PCOS but normal blood results
- Your GP needs to rule out other ovarian conditions
- The diagnosis remains unclear after initial testing
The scan looks for polycystic ovaries, defined as having 12 or more follicles (2-9mm diameter) in each ovary or an ovarian volume greater than 10ml.
What Happens After PCOS Diagnosis?
Once diagnosed, your GP may treat you directly or refer you to a specialist - either a gynaecologist or endocrinologist, depending on your primary symptoms and local protocols.
Immediate Next Steps
- Lifestyle counseling: Guidance on diet, exercise, and weight management
- Symptom management: Treatment plans for irregular periods, excess hair growth, or fertility concerns
- Long-term monitoring: Annual blood pressure checks and diabetes screening
- Specialist referral: If symptoms are complex or don't respond to initial treatment
Understanding how nutrition affects PCOS symptoms becomes crucial at this stage, as dietary changes often form the foundation of effective management.
Common Challenges in Getting a PCOS Diagnosis
Symptoms Being Dismissed
Research shows that over 60% of women experienced difficulties receiving a PCOS diagnosis, with many reporting their symptoms were minimized or attributed to other causes.
Long Waiting Times
NHS data indicates significant variation in access to specialist PCOS services across different regions, with 95% of women finding it difficult to access specialized PCOS services within the NHS.
Incomplete Testing
Some GPs may not be familiar with the full range of tests required, potentially leading to missed diagnoses or delays.
Red Flag Symptoms: Seek immediate evaluation if you experience rapid onset of symptoms, severe virilization (deep voice, male-pattern balding), or sudden dramatic changes, as these may indicate androgen-secreting tumors requiring urgent assessment.
Advocating for Yourself in the NHS System
Know Your Rights
- You have the right to a second opinion if diagnosis is unclear
- You can request specialist referral if symptoms significantly impact your life
- You're entitled to see test results and have them explained clearly
- You can choose which hospital to be referred to under NHS Choose and Book
Preparing for Appointments
Maximize appointment effectiveness by:
- Writing down symptoms and questions beforehand
- Bringing a support person if helpful
- Requesting written summaries of discussions and next steps
- Asking for copies of all test results
PCOS Diagnosis in Special Circumstances
Adolescents and Young Women
NHS guidelines recommend caution when diagnosing PCOS in teenagers, as irregular periods are common after menarche. Workup is typically delayed until at least two years of oligomenorrhea, and some guidelines suggest all three Rotterdam criteria should be met before diagnosis in this age group.
Women Over 40
PCOS diagnosis becomes more complex approaching menopause, as normal hormonal changes can mimic or mask PCOS symptoms. Additional testing may be needed to differentiate between PCOS and perimenopausal changes.
Women Trying to Conceive
If fertility is a primary concern, your GP may refer you directly to a fertility specialist or reproductive endocrinologist for comprehensive evaluation and treatment planning.
Supporting Your PCOS Journey with Nutrition
While pursuing diagnosis, focusing on PCOS-friendly nutrition strategies can help manage symptoms. Many women find that dietary changes improve energy levels, regulate cycles, and support weight management even before formal treatment begins.
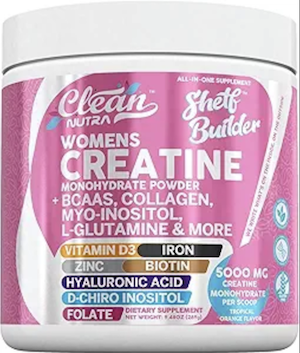 Quality supplements like creatine can also support overall health during the diagnosis process, with emerging research suggesting benefits for insulin sensitivity and lean muscle mass in women with PCOS.
Quality supplements like creatine can also support overall health during the diagnosis process, with emerging research suggesting benefits for insulin sensitivity and lean muscle mass in women with PCOS.
Regional Variations in PCOS Care
PCOS care quality varies significantly across UK regions. Some areas have dedicated PCOS clinics with multidisciplinary teams, while others rely primarily on general gynecology or endocrinology services.
Research your local Clinical Commissioning Group's guidelines and services to understand what's available in your area.
What to Expect After Diagnosis
Following confirmation of PCOS, your care team will typically focus on:
- Symptom prioritization: Addressing your most troublesome symptoms first
- Metabolic screening: Regular monitoring for diabetes and cardiovascular risk factors
- Fertility planning: Discussions about current and future pregnancy plans
- Long-term health: Education about increased risks and prevention strategies
Many women find that having a confirmed diagnosis brings relief and validation, even when symptoms have been present for years.
Conclusion
Getting a pcos diagnosis in the UK requires persistence, preparation, and knowledge of the system. While challenges exist, understanding the Rotterdam criteria, knowing what tests to expect, and advocating effectively for yourself significantly improves your chances of timely, accurate diagnosis.
Remember that PCOS is a lifelong condition requiring ongoing management, but with proper diagnosis and treatment, most women can effectively manage their symptoms and lead healthy, fulfilling lives. The key is getting started with the right diagnosis and building a supportive healthcare team.
If you're struggling with suspected PCOS symptoms, don't give up. Your symptoms are real, valid, and deserving of proper medical attention. With the right approach and persistence, you can get the diagnosis and care you need.

Community Comments
Community Comments
Add a comment