Living with Polycystic Ovary Syndrome (PCOS) presents numerous challenges beyond irregular periods and hormone imbalances. One critical yet often overlooked aspect is its powerful connection to mental health.
Research conclusively shows women with PCOS are three times more likely to experience depression compared to those without the condition. Understanding this link isn't just helpful—it's essential for effective treatment of both conditions.

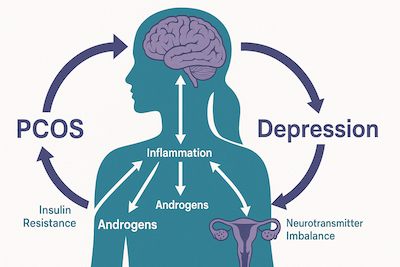
The bidirectional relationship between PCOS and depression showing hormonal, inflammatory, and psychological pathways
The PCOS-Depression Connection: What Science Reveals
The relationship between PCOS and depression isn't coincidental—it's rooted in biology and psychology. Recent research has identified several pathways that explain why these conditions frequently co-occur:
Biological Mechanisms: How PCOS Affects Brain Chemistry
- Hormonal Imbalances: Elevated androgens (male hormones) in PCOS directly impact neurotransmitter function, particularly serotonin and dopamine—key mood regulators
- Insulin Resistance: Present in up to 80% of women with PCOS, insulin resistance affects glucose metabolism in the brain, altering energy availability to brain cells
- Chronic Inflammation: Studies in the Journal of Clinical Endocrinology & Metabolism demonstrate that systemic inflammation in PCOS affects the hypothalamic-pituitary-adrenal (HPA) axis, disrupting stress response and mood regulation
- Cortisol Dysregulation: Many women with PCOS show abnormal cortisol patterns, which strongly correlate with depressive symptoms
Psychological Factors: The Emotional Burden of PCOS
- Body Image Concerns: Managing visible symptoms like weight gain, acne, and hirsutism (excessive hair growth) creates significant psychological distress
- Fertility Challenges: The uncertainty around conception can trigger profound grief, anxiety, and feelings of inadequacy
- Symptom Unpredictability: The unpredictable nature of PCOS symptoms creates ongoing stress and feeling of loss of control
- Social Isolation: Many women withdraw from social situations due to physical symptoms or emotional distress
This creates a bidirectional relationship where each condition can trigger or worsen the other.
Research published in 2023 in the journal Frontiers in Endocrinology found that treating depression in women with PCOS improved metabolic parameters, while addressing insulin resistance often alleviated depressive symptoms—confirming the interconnected nature of these conditions.
PCOS and Depression: By the Numbers
- Women with PCOS have a 3x higher risk of developing major depressive disorder
- 40-60% of women with PCOS experience depressive symptoms at clinical or subclinical levels
- Depression risk remains elevated by 2x even after controlling for obesity and other factors
- The average age of depression onset is 3-4 years earlier in women with PCOS
- Only 25% of women with PCOS are screened for depression during treatment
Recognizing Depression When You Have PCOS
Depression symptoms in women with PCOS may present differently than typical depression, and many symptoms overlap with PCOS itself, making identification challenging. Be alert to these warning signs:
| Symptom | How It Presents in PCOS with Depression | How It Differs from PCOS Alone |
|---|---|---|
| Persistent Sadness | Feelings of emptiness or hopelessness lasting more than two weeks, often unrelated to specific PCOS symptoms | More pervasive than occasional frustration about PCOS symptoms; doesn't improve even when PCOS symptoms are better managed |
| Anhedonia | Loss of interest in previously enjoyed activities, including those unrelated to physical appearance or health | Goes beyond avoiding activities due to PCOS symptoms; affects areas of life not directly impacted by PCOS |
| Sleep Changes | Insomnia or hypersomnia (excessive sleep) that persists regardless of menstrual cycle phase | More severe than the sleep disruptions caused by hormonal fluctuations or night sweats associated with PCOS |
| Energy Levels | Profound fatigue and lack of energy not relieved by rest | More severe than the typical tiredness associated with PCOS; present even when other PCOS symptoms are well-controlled |
| Appetite/Weight | Significant changes in appetite and weight unrelated to PCOS management efforts | Weight changes occur despite consistent diet and exercise; may include weight loss (which is less common in PCOS alone) |
| Cognitive Function | Difficulty concentrating, making decisions, or remembering details | More severe than the "brain fog" sometimes reported with PCOS; impacts daily functioning |
| Self-Worth | Persistent feelings of worthlessness or excessive guilt | Goes beyond frustration about specific PCOS symptoms; includes negative self-evaluation in areas unrelated to PCOS |
| Suicidal Thoughts | Thoughts of death or suicide | Requires immediate attention regardless of PCOS status |
Important: If you experience thoughts of suicide or self-harm, seek immediate help from a healthcare provider, call the National Suicide Prevention Lifeline at 988 (US), or text HOME to 741741 to reach the Crisis Text Line.
These resources are available 24/7, and reaching out shows strength, not weakness.
7 Evidence-Based Treatment Approaches for PCOS and Depression
Managing both conditions simultaneously creates a powerful synergistic effect where improvements in one area positively impact the other. Research supports these approaches:
1. Medical Interventions That Address Both Conditions
Antidepressants and PCOS
Selective Serotonin Reuptake Inhibitors (SSRIs) can effectively treat depression in women with PCOS, with some additional considerations:
- Research-backed options: Fluoxetine and sertraline have been studied specifically in PCOS populations
- Metabolic benefits: Some research suggests certain SSRIs may help modulate insulin sensitivity
- Considerations: Discuss potential side effects like weight changes with your provider, as these can impact PCOS management
Hormone Management
Regulating hormones can improve mood by addressing underlying imbalances:
- Combined oral contraceptives: Particularly those with anti-androgenic properties can improve both PCOS symptoms and mood
- Anti-androgen medications: Drugs like spironolactone may help with both physical symptoms and mood by reducing testosterone levels
Insulin-Sensitizing Approaches
Addressing insulin resistance can improve both metabolic health and mood regulation:
- Metformin: Improves insulin sensitivity and may have direct mood benefits
- Inositol supplements: Particularly myo-inositol and D-chiro-inositol in a 40:1 ratio have shown benefits for both insulin sensitivity and mood
- Berberine: Some studies suggest benefits for insulin resistance and inflammation in PCOS
2. Nutrition Strategies That Target Both PCOS and Depression
Diet profoundly affects both conditions through multiple pathways:
- Anti-inflammatory eating patterns: Mediterranean and DASH diets show benefits for both conditions by reducing inflammation
- Blood sugar regulation: Following a low-glycemic diet helps prevent insulin spikes and crashes that affect both hormones and mood
- Omega-3 fatty acids: Found in fatty fish, walnuts, and flaxseeds, these have established benefits for depression and may reduce inflammation in PCOS
- Gut microbiome support: Emerging research suggests probiotics and prebiotic foods may benefit both conditions
For specific dietary guidance, explore our articles on low-glycemic fruits and vegetarian PCOS diet options.
3. Exercise Interventions With Dual Benefits
Physical activity powerfully addresses both conditions:
- Mood enhancement: Exercise releases endorphins and increases BDNF (Brain-Derived Neurotrophic Factor), which supports brain health and mood regulation
- Insulin sensitivity: Regular activity improves cellular response to insulin, addressing a core PCOS issue
- Stress reduction: Physical activity reduces cortisol levels and improves stress resilience
- Sleep quality: Regular exercise promotes better sleep, which benefits both conditions
PCOS-Depression Exercise Prescription
Research suggests this combination provides optimal benefits for both conditions:
- Moderate aerobic activity: 30 minutes, 3-5 times weekly (walking, swimming, cycling)
- Strength training: 2-3 sessions weekly, focusing on major muscle groups
- Mind-body exercise: Yoga or tai chi 1-2 times weekly for stress reduction
- For low motivation days: Even 10-minute movement sessions provide benefits
Note: Start where you are. If depression makes exercise challenging, begin with 5-10 minute sessions and gradually increase duration and intensity.
4. Therapeutic Approaches for Psychological Support
Mental health therapies provide crucial support:
- Cognitive Behavioral Therapy (CBT): Particularly effective for women with PCOS and depression by addressing negative thought patterns about body image, fertility, and health challenges
- Mindfulness-Based Cognitive Therapy (MBCT): Combines mindfulness practices with cognitive therapy, showing good results for preventing depression relapse
- Acceptance and Commitment Therapy (ACT): Helps women develop psychological flexibility around chronic health conditions
- Group therapy: Provides validation, reduces isolation, and offers practical coping strategies
5. Stress Management and Resilience Building
Chronic stress worsens both PCOS and depression through multiple pathways:
- HPA axis modulation: Stress reduction techniques help normalize cortisol patterns
- Inflammatory reduction: Regular relaxation practices can lower inflammatory markers
- Emotional regulation: Developing healthy coping strategies improves resilience
Effective techniques include:
- Mindfulness meditation (even 10 minutes daily shows benefits)
- Deep breathing exercises
- Progressive muscle relaxation
- Nature exposure ("forest bathing" has research-backed benefits)
- Journaling for emotional processing
6. Sleep Optimization for Hormonal and Mood Balance
Poor sleep creates a vicious cycle with both PCOS and depression:
- Insulin sensitivity: Sleep loss increases insulin resistance
- Hormone regulation: Sleep disruption affects reproductive hormones
- Mood regulation: Poor sleep is a major risk factor for depression
- Inflammation: Sleep deprivation increases inflammatory markers
Effective strategies include:
- Maintaining consistent sleep-wake times
- Creating a cool, dark sleeping environment
- Limiting screen time before bed
- Establishing a relaxing bedtime routine
- Considering supplements like magnesium or melatonin (with healthcare provider approval)
7. Building a Comprehensive Support System
Managing both PCOS and depression requires holistic support:
Your Ideal Support Team
- Medical providers: Endocrinologist or gynecologist specializing in PCOS, psychiatrist or primary care provider for depression management
- Mental health professionals: Therapist, counselor, or psychologist experienced with chronic health conditions
- Allied health professionals: Registered dietitian familiar with PCOS, exercise physiologist
- Community support: PCOS support groups, depression support groups, online communities
- Personal connections: Friends and family who understand your challenges
Communication between team members is key to coordinated care addressing both conditions simultaneously.
Breaking the Cycle: Your Practical Action Plan
Taking concrete steps is essential for managing both conditions effectively:
- Track your symptoms: Start a journal documenting both PCOS and mood symptoms to identify patterns and triggers
- Prioritize consistent care: Schedule regular check-ins with both your PCOS provider and mental health professional
- Implement gradual dietary changes: Add one anti-inflammatory food daily, such as berries, fatty fish, or pumpkin seeds
- Create a movement routine: Start with just 10 minutes of walking daily and gradually increase
- Develop a sleep hygiene protocol: Establish consistent bedtime and morning routines
- Practice daily stress reduction: Even 5 minutes of deep breathing can help
- Build your knowledge base: Educate yourself about both conditions through reliable sources
- Connect with others: Join support groups specifically for women managing both PCOS and depression
- Practice self-compassion: Recognize that managing these conditions is challenging and be kind to yourself during difficult periods
"For years I treated my PCOS and depression as completely separate issues, seeing different doctors who never communicated with each other. When I finally found providers who understood the connection, everything changed. Addressing my insulin resistance actually improved my depression symptoms, while treating my depression gave me the emotional energy to better manage my PCOS. It's not always easy, but understanding they're connected has made managing both so much more effective."
Frequently Asked Questions About PCOS and Depression
Can PCOS directly cause depression?
Yes, PCOS can directly contribute to depression through multiple mechanisms. The hormonal imbalances characteristic of PCOS—particularly elevated testosterone and insulin resistance—can affect neurotransmitter function and brain chemistry.
Research published in the Journal of Affective Disorders shows that inflammation associated with PCOS impacts brain regions involved in mood regulation.
Additionally, managing chronic symptoms like irregular periods, weight gain, hair growth, and fertility challenges creates significant psychological burden. This combination of biological and psychological factors creates a direct pathway between PCOS and depression. Tweet this
Do antidepressants affect PCOS symptoms?
Antidepressants can have mixed effects on PCOS symptoms. Some selective serotonin reuptake inhibitors (SSRIs) may slightly improve insulin sensitivity in certain women, potentially helping with metabolic aspects of PCOS.
However, some antidepressants might contribute to weight gain, which could temporarily worsen insulin resistance. The most important consideration is that effectively treating depression improves your ability to manage PCOS through lifestyle modifications and medical treatment adherence.
Work with healthcare providers who understand both conditions to find the medication that best balances mental health needs with PCOS management. Tweet this
What dietary changes help both PCOS and depression?
An anti-inflammatory, low-glycemic diet benefits both PCOS and depression by reducing systemic inflammation that contributes to both conditions. Focus on omega-3 rich foods like fatty fish, walnuts, and flaxseeds, which support brain health and reduce inflammation.
Include plenty of fiber from vegetables, legumes, and sweet potatoes to stabilize blood sugar. Limit refined carbohydrates and sugars that cause blood sugar spikes and crashes affecting mood and hormones.
Some women find that reducing dairy and gluten improves both conditions, though evidence is mixed. Consider vegetarian PCOS diet options that emphasize plant-based proteins and anti-inflammatory foods. Tweet this
How does exercise impact both PCOS and depression?
Regular physical activity offers powerful benefits for both conditions. For PCOS, exercise improves insulin sensitivity, reduces testosterone levels, and helps with weight management.
For depression, it increases endorphins (natural mood elevators), boosts brain-derived neurotrophic factor (BDNF) that supports brain health, reduces inflammation, and improves sleep quality.
A combination of moderate aerobic exercise (like walking, swimming, or cycling) 3-5 times weekly for 30 minutes, plus strength training 2-3 times weekly, provides optimal benefits. Even 10-minute movement sessions throughout the day can help when energy and motivation are low due to depression.
Can managing stress improve both PCOS and depression symptoms?
Yes, stress management is a powerful intervention for both conditions. Chronic stress elevates cortisol, which worsens insulin resistance in PCOS and depletes mood-regulating neurotransmitters in depression.
Effective stress reduction techniques include mindfulness meditation, yoga, deep breathing exercises, progressive muscle relaxation, and spending time in nature.
Studies show that regular practice of these techniques can reduce cortisol levels by 10-25%, improving both hormonal balance and mood regulation. Even 5-10 minutes of daily practice can produce noticeable benefits when done consistently. Tweet this
Should I tell my PCOS doctor about my depression symptoms?
Absolutely yes. Open communication between all your healthcare providers is essential for comprehensive care. Your PCOS symptoms and depression may be biochemically linked, and treatments for one condition can affect the other.
Additionally, depressive symptoms might be mistaken for PCOS-related fatigue or vice versa, leading to incomplete treatment. When your providers understand the full picture, they can coordinate care more effectively, potentially adjusting treatments to address both conditions simultaneously.
Don't hesitate to bring up mood concerns with your PCOS provider, as they're an important part of your overall health picture. Tweet this
How do I know if my depression is related to PCOS or something else?
It can be difficult to determine the exact relationship between your PCOS and depression, as they often influence each other.
Some clues that your depression may be strongly connected to PCOS include: mood symptoms that fluctuate with your menstrual cycle or PCOS symptom flares; depression that began or worsened around the time of your PCOS diagnosis; mood improvements when PCOS symptoms are better controlled; or depression that hasn't fully responded to traditional treatments.
However, these are just patterns, not definitive indicators. The most important approach is to treat both conditions comprehensively, regardless of which came first. A mental health professional familiar with PCOS can help determine the most appropriate treatment approach. Tweet this
Summary: Creating Your PCOS and Depression Management Plan
Breaking the cycle between PCOS and depression requires a comprehensive approach that addresses both conditions simultaneously.
By understanding the biological connections and implementing evidence-based strategies, you can create a powerful healing synergy where improvements in one condition positively impact the other.
Remember that managing these interconnected conditions is a journey that requires patience and consistent effort. There may be setbacks along the way, but with the right support system and treatment approaches, you can significantly improve both your physical and mental well-being.
The most important first step is acknowledging the connection between these conditions and seeking providers who understand this relationship. From there, you can build a personalized plan incorporating the strategies outlined in this article, adapting them to your specific needs and situation.
Expert Tip: Create a one-page "PCOS and Depression Management Plan" that you can share with all your healthcare providers. Include your current symptoms, medications, supplements, lifestyle strategies, and goals.
This helps ensure coordinated care and gives you a clear roadmap for managing both conditions effectively.
How This Article Was Made
This article was created through a comprehensive review of medical literature on PCOS, depression, and their interconnection. We consulted peer-reviewed studies, clinical guidelines, and interviews with specialists in both reproductive endocrinology and mental health.
Key sources included:
- Research on PCOS and depression comorbidity from the Journal of Clinical Endocrinology & Metabolism, Journal of Affective Disorders, and Frontiers in Endocrinology
- Clinical practice guidelines from the Endocrine Society and the American Psychiatric Association
- Systematic reviews and meta-analyses on treatment approaches for both conditions
- Input from healthcare providers specializing in PCOS and mental health
We strive to provide accurate, evidence-based information that acknowledges both the biological and psychological aspects of these conditions while offering practical, actionable strategies for improving quality of life.
Community Comments
Community Comments
Add a comment