What is Glycemic Index? A Simple Explanation
The glycemic index is a ranking system that measures how quickly foods containing carbohydrates raise blood sugar levels. Foods are ranked on a scale from 0 to 100, with higher numbers indicating foods that cause faster and higher spikes in blood sugar.
Think of the glycemic index as a "speed rating" for how rapidly a food turns into glucose in your bloodstream:
- Low GI foods (55 or less): Digest slowly, causing a gradual, modest rise in blood sugar
- Medium GI foods (56-69): Cause moderate blood sugar increases
- High GI foods (70 or above): Digest quickly, causing rapid spikes in blood sugar
Why Glycemic Index Matters for PCOS
For women with PCOS, understanding glycemic index is particularly important because:
- Up to 80% of women with PCOS have insulin resistance, where your body doesn't respond properly to insulin
- Blood sugar spikes trigger excess insulin production
- Higher insulin levels can worsen hormone imbalances that drive PCOS symptoms like irregular periods, acne, and unwanted hair growth
- Managing blood sugar stability can improve fertility, energy levels, and weight management
By focusing on low glycemic index foods, you can help keep your blood sugar more stable, which may reduce insulin resistance and improve many PCOS symptoms over time.
How Glycemic Index Works in Your Body
When you eat carbohydrates, your digestive system breaks them down into glucose (sugar), which enters your bloodstream. Your pancreas then releases insulin, a hormone that helps move glucose from your blood into your cells for energy.
With high GI foods, this process happens rapidly, causing:
- A quick surge of glucose into your bloodstream
- A large release of insulin to manage the glucose
- Often followed by a "crash" in blood sugar and energy
Low GI foods, on the other hand, are digested and absorbed more slowly, resulting in a more gradual rise in blood glucose and a more moderate insulin response—exactly what's beneficial for PCOS management.
Factors That Affect a Food's Glycemic Index
Several factors influence where a food falls on the glycemic index scale:
- Fiber content: Higher fiber slows digestion, lowering GI
- Fat and protein content: These nutrients slow carbohydrate absorption
- Food processing: More processed foods typically have higher GI
- Ripeness: Riper fruits have higher GI values
- Cooking method and time: Longer cooking can break down fiber and raise GI
- Acidity: Acidic foods like vinegar or lemon juice can lower the GI of a meal
Common Foods and Their Glycemic Index
Here's a quick reference guide to common foods and their glycemic index values:
Low GI Foods (55 or less)
- Most non-starchy vegetables (broccoli, cauliflower, leafy greens)
- Most fruits (apples, berries, pears, oranges)
- Legumes (lentils, chickpeas, beans)
- Steel-cut or rolled oats
- Quinoa
- Greek yogurt (unsweetened)
- Nuts and seeds
Medium GI Foods (56-69)
- Brown rice
- Whole wheat bread
- Sweet potatoes
- Ripe bananas
- Basmati rice
- Couscous
High GI Foods (70 or above)
- White bread
- White rice
- Regular potatoes
- Most breakfast cereals
- Rice cakes
- Watermelon
- Sugary beverages
For a more detailed breakdown of foods and their GI values, check out our comprehensive glycemic index chart.
Beyond the Number: Glycemic Load
While glycemic index is useful, it doesn't tell the whole story. Glycemic load (GL) considers both the quality (GI) and quantity (portion size) of carbohydrates:
Glycemic Load = (GI × carbohydrate content in grams) ÷ 100
For example, watermelon has a high GI (around 80) but contains relatively few carbs per serving, giving it a lower glycemic load. This means a typical portion won't impact your blood sugar as dramatically as its high GI might suggest.
- Low GL: 10 or less
- Medium GL: 11-19
- High GL: 20 or more
For women with PCOS, paying attention to glycemic load can provide a more practical approach to meal planning than focusing solely on glycemic index.
Practical Tips for Using Glycemic Index with PCOS
Here are some actionable ways to apply glycemic index knowledge to your PCOS management:
- Pair higher GI foods with protein, fat, or fiber to slow digestion and reduce blood sugar impact
- Add vinegar to meals (like in salad dressing) to lower the glycemic response
- Choose whole grains over refined options for more stable blood sugar
- Eat fruits with the skin on when possible for extra fiber
- Include protein with each meal and snack to balance blood sugar
- Experiment with sourdough bread, which typically has a lower GI than regular bread
- Cook pasta al dente rather than soft to lower its GI
- Try meal planning services like PCOS Meal Planner that focus on low GI options
Remember, you don't need to eliminate all higher GI foods completely. Instead, focus on balance, portion control, and making swaps when possible to create meals that support steady blood sugar levels.
How to Start a Low Glycemic Diet for PCOS
you're ready to incorporate glycemic index awareness into your PCOS management, here's a simple way to begin:- Start with breakfast: Replace high GI breakfast options (sugary cereals, white toast) with lower GI alternatives like Greek yogurt with berries and nuts, or overnight oats
- Make one swap at a time: Try brown rice instead of white, sweet potatoes instead of regular potatoes, or whole grain bread instead of white bread
- Add a source of protein and healthy fat to each meal and snack
- Increase your vegetable intake: Most non-starchy vegetables have minimal impact on blood sugar
- Be mindful of portion sizes for higher GI foods
- Track your symptoms to notice improvements as you make dietary changes
For more comprehensive guidance, check out our Ultimate Guide to Low Glycemic Index Foods for PCOS.
Combining Glycemic Index Knowledge with Other PCOS Strategies
While focusing on low glycemic index foods can significantly help manage PCOS symptoms, it works best as part of a comprehensive approach. Consider combining your low GI eating pattern with:
- Regular physical activity: Exercise improves insulin sensitivity and complements a low GI diet
- Stress management: Chronic stress can raise blood sugar levels
- Adequate sleep: Poor sleep affects insulin sensitivity and hunger hormones
- Supplements: Some supplements like inositol, chromium, and creatine
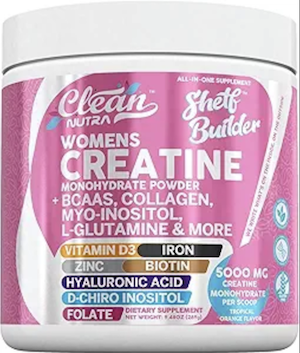 may support insulin sensitivity
may support insulin sensitivity - Hydration: Staying well-hydrated supports overall metabolic health
Frequently Asked Questions About Glycemic Index and PCOS
How quickly will switching to low GI foods improve my PCOS symptoms?
While everyone's body responds differently, many women notice improvements in energy levels and reduced cravings within 1-2 weeks of consistently choosing lower GI foods.
Improvements in other symptoms like irregular periods, acne, or unwanted hair growth typically take longer—often 2-3 months or more of consistent dietary changes.
Remember that the glycemic index is just one tool in PCOS management, and combining it with other lifestyle approaches often yields the best results. Tweet this
Do I need to completely avoid high GI foods with PCOS?
No, you don't need to completely eliminate high GI foods. The glycemic index is best used as a guide rather than a strict rule. What matters most is your overall dietary pattern and the context of how you eat higher GI foods.
For example, enjoying a small portion of a higher GI food as part of a balanced meal that includes protein, healthy fats, and fiber will have less impact on your blood sugar than eating that same food alone.
Focus on making lower GI choices most of the time while allowing occasional higher GI foods in moderation. Tweet this
Is glycemic index more important than counting calories for PCOS?
For many women with PCOS, focusing on glycemic index and overall food quality tends to be more beneficial than strict calorie counting.
This is because insulin resistance—a common feature of PCOS—responds better to the quality of carbohydrates (measured by GI) than simply reducing total calories. That said, energy balance still matters.
The ideal approach for most women with PCOS is to prioritize low GI, nutrient-dense foods while being mindful of portion sizes and overall energy intake. This combined strategy addresses both insulin resistance and weight management without the need for strict calorie counting. Tweet this
Can vegetarians and vegans with PCOS still follow a low GI diet?
Absolutely! Plant-based diets can be excellent for managing PCOS symptoms and are completely compatible with low GI eating. Plant proteins like legumes (beans, lentils, chickpeas) are naturally low GI and high in fiber, making them ideal for blood sugar management.
Other plant-based, low GI foods include most vegetables, many fruits, nuts, seeds, and whole grains like quinoa and steel-cut oats. For more specific guidance, check out our Plant-Based Low GI Guide for PCOS. Tweet this
How does glycemic index relate to insulin resistance in PCOS?
Glycemic index and insulin resistance are closely connected, especially in PCOS. When you consume high GI foods, they cause rapid spikes in blood sugar, which trigger your pancreas to release large amounts of insulin.
For the estimated 70-80% of women with PCOS who have insulin resistance, the body doesn't respond efficiently to this insulin, leading to even higher insulin levels as the body tries to compensate.
These chronically elevated insulin levels then worsen hormonal imbalances by stimulating the ovaries to produce more androgens (male hormones), which drive many PCOS symptoms.
By choosing low GI foods, you can help maintain more stable blood sugar levels, reduce insulin demands, and gradually improve insulin sensitivity—addressing one of the root causes of PCOS symptoms. For more information, see our guide on Insulin-Resistant PCOS: Complete Food Guide. Tweet this

Community Comments
Community Comments
Add a comment