Undiagnosed PCOS: The Silent Epidemic Affecting Millions
Polycystic Ovary Syndrome (PCOS) is the most common hormonal disorder among women of reproductive age, affecting approximately 8-13% of women worldwide. Yet shockingly, up to 70% of women with PCOS remain undiagnosed.
This means millions of women are struggling with unexplained symptoms, facing health complications, and missing opportunities for effective treatment—all because their PCOS has gone unrecognized.
In this article, we'll explore why PCOS is so frequently overlooked, the subtle signs that might indicate undiagnosed PCOS, and what steps you can take to advocate for proper testing and care.
The Scope of Undiagnosed PCOS: More Common Than You Think
The statistics surrounding undiagnosed PCOS are sobering:
- Studies estimate that 50-70% of women with PCOS are undiagnosed
- The average woman sees 3-4 different doctors before receiving a correct diagnosis
- Many women wait 2+ years from symptom onset to diagnosis
- Diagnosis delays are even longer for women of color and those in underserved communities
These numbers represent real women experiencing real symptoms—women who often blame themselves for issues like weight gain, irregular periods, or mood changes without realizing there's an underlying medical condition that explains their experiences.
Why Is PCOS So Frequently Missed?
Several factors contribute to the high rates of undiagnosed PCOS:
1. Variable Symptom Presentation
No two cases of PCOS look exactly alike. The syndrome manifests differently in each woman, making it difficult to recognize from a standard symptom checklist.
While some women experience the "classic" signs like irregular periods, excess hair growth, and weight gain, others might have more subtle symptoms or a completely different combination of signs.
2. Fragmented Healthcare Systems
Women often see different specialists for different symptoms: a dermatologist for acne, an endocrinologist for metabolic issues, a gynecologist for menstrual irregularities. Without a coordinated approach, the big picture—PCOS—can be missed as each doctor focuses only on their specialty.
3. Dismissal of Women's Health Concerns
Research consistently shows that women's pain and symptoms are more likely to be dismissed or downplayed in medical settings.
Symptoms like irregular periods or trouble losing weight may be attributed to stress, lifestyle, or even just "being a woman" rather than investigated as potential signs of a hormonal disorder.
4. Lack of Provider Education
Many healthcare providers receive minimal training on PCOS, especially its more subtle presentations. Without updated knowledge on diagnostic criteria and management options, clinicians may miss cases that don't fit the most obvious profile.
5. The Name Itself Is Misleading
The term "polycystic ovary syndrome" suggests that ovarian cysts are the defining feature. However, many women with PCOS don't have visible cysts on ultrasound, while some women without PCOS do have ovarian cysts. This nomenclature creates confusion for both patients and providers.

Support your hormonal health naturally! While seeking proper diagnosis is crucial, natural approaches can also help manage PCOS symptoms. Rosemary has anti-inflammatory properties that may help with hormone balance. Try this rosemary water as a refreshing addition to your PCOS management routine.
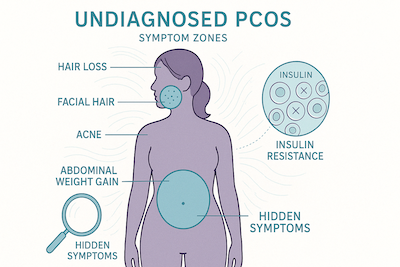
Hidden Signs of PCOS You Might Be Missing
While many people associate PCOS with obvious symptoms like missed periods and excessive hair growth, the syndrome can manifest in subtle ways that are easily attributed to other causes:
Metabolic Symptoms
- Unexplained weight gain or difficulty losing weight, especially around the abdomen
- Intense hunger or cravings, particularly for carbohydrates
- Fatigue or energy crashes after meals
- Darkened skin patches (acanthosis nigricans) in body folds like the neck, armpits, or groin
These symptoms are often related to insulin resistance, which affects up to 70% of women with PCOS. Understanding the glycemic impact of foods becomes especially important, as we discuss in articles like low glycemic desserts and the glycemic index of different fruits.
Skin and Hair Symptoms
- Adult acne that flares up cyclically or doesn't respond to typical treatments
- Hair thinning or hair loss on the scalp, often at the crown or in a male-pattern distribution
- Fine, dark hair growth on the face, chest, or back (hirsutism)
- Skin tags, especially around the neck or armpits
- Oily skin or scalp despite appropriate skincare
These symptoms stem from hormonal imbalances, particularly elevated androgens (male hormones). Resources like rosemary water for PCOS hair loss address these specific concerns.
Menstrual and Reproductive Symptoms
- Irregular periods (either infrequent or too frequent)
- Very heavy periods alternating with light periods
- Prolonged periods lasting more than 7 days
- Unexplained infertility or difficulty conceiving
- Recurrent early miscarriages
Mood and Cognitive Symptoms
- Mood swings that seem out of proportion or unrelated to circumstances
- Anxiety or depression that worsens at certain times of the month
- Brain fog or difficulty concentrating
- Sleep disturbances despite good sleep hygiene
These symptoms are often dismissed as "just stress" or "hormones being hormones," but they can significantly impact quality of life and deserve proper attention and treatment.
The Different "Types" of PCOS Presentations
While not official medical categories, understanding the four common patterns of PCOS can help identify which type you might have:
1. "Classic" PCOS
This presentation includes most of the well-known symptoms: irregular periods, elevated androgens (causing symptoms like excess hair growth), and polycystic ovaries visible on ultrasound. Women with this type often struggle with weight management and show clear signs of insulin resistance.
2. "Lean" PCOS
Women with lean PCOS maintain a normal or low BMI but still experience hormonal symptoms. This type is frequently missed because healthcare providers often associate PCOS with obesity. However, these women still have hormonal imbalances and can face fertility challenges.
3. "Inflammatory" PCOS
This presentation is characterized by chronic inflammation, which may be detected through blood tests showing elevated inflammatory markers. Women with this type often experience fatigue, joint pain, headaches, and digestive issues alongside hormonal symptoms.
4. "Post-Pill" PCOS
Some women develop PCOS-like symptoms after stopping hormonal birth control. For some, these symptoms resolve within a few months as the body readjusts, but for others, they persist and may reflect previously masked PCOS. For more information, see our article on post-birth control PCOS diet.
The Real Impact of Undiagnosed PCOS
Going without a proper PCOS diagnosis doesn't just mean living with uncomfortable symptoms—it can have far-reaching health implications:
Short-Term Impacts
- Reduced quality of life due to physical symptoms
- Mental health challenges like anxiety and depression
- Fertility difficulties without understanding the cause
- Weight management struggles that don't respond to conventional approaches
Long-Term Health Risks
- Type 2 diabetes: Women with PCOS have 5-7 times higher risk
- Cardiovascular disease: Higher rates of high blood pressure, cholesterol abnormalities, and heart disease
- Endometrial cancer: Increased risk due to irregular menstrual cycles
- Fatty liver disease: More common in women with unmanaged PCOS
- Sleep apnea: 5-10 times more prevalent in women with PCOS
With proper diagnosis and management, many of these risks can be significantly reduced, which is why identifying PCOS early is so important.
When to Suspect PCOS and Seek Testing
Consider seeing a healthcare provider for PCOS evaluation if you experience:
- Fewer than 9 menstrual periods per year or cycles longer than 35 days
- Significant hair growth in areas where women typically don't grow hair (face, chest, back)
- Severe acne that doesn't respond to conventional treatments
- Gradual hair thinning or hair loss on your scalp
- Unexplained weight gain, especially around your abdomen
- Difficulty getting pregnant after trying for 12 months (or 6 months if over 35)
- Symptoms of insulin resistance (fatigue after meals, intense carb cravings, darkened skin patches)
The more symptoms you have, the more important it is to get evaluated, even if each individual symptom seems mild.
Advocating for Proper Diagnosis: What Tests to Request
If you suspect you have PCOS, these are the key tests to discuss with your healthcare provider:
Hormonal Blood Tests
- Testosterone (total and free): Often elevated in PCOS
- DHEAS: Another androgen that may be high
- Sex hormone binding globulin (SHBG): Often low in PCOS
- LH and FSH: These pituitary hormones often show an abnormal ratio in PCOS
- Anti-Müllerian hormone (AMH): Typically elevated in PCOS
Metabolic Tests
- Fasting glucose: To check for prediabetes
- Fasting insulin: To assess insulin resistance (often overlooked!)
- HbA1c: Shows average blood sugar over the past 3 months
- Glucose tolerance test: More comprehensive way to assess insulin resistance
- Lipid panel: To check cholesterol levels
Imaging
- Transvaginal ultrasound: To check for polycystic ovaries
Ruling Out Other Conditions
- Thyroid function tests: Hypothyroidism can mimic some PCOS symptoms
- Prolactin: Elevated levels suggest different pituitary conditions
- 17-hydroxyprogesterone: To rule out certain forms of adrenal hyperplasia
- Cortisol: To check for Cushing's syndrome
Remember, PCOS is diagnosed when other potential causes have been ruled out and at least two of the following criteria are met:
- Irregular or absent periods
- Clinical signs of high androgens (like excess hair growth) or blood tests showing elevated androgens
- Polycystic ovaries on ultrasound
Finding the Right Healthcare Provider
Not all healthcare providers have the same experience with PCOS. Consider:
- Endocrinologists: Specialists in hormonal disorders who may have the most comprehensive understanding of PCOS
- Reproductive endocrinologists: Particularly helpful if fertility is a concern
- Gynecologists with PCOS focus: Some gynecologists develop expertise in this area
- Functional medicine practitioners: May offer more holistic approaches alongside conventional testing
When selecting a provider, don't hesitate to ask about their experience with PCOS and their approach to diagnosis and treatment. A good provider will:
- Listen to your concerns without dismissing them
- Order comprehensive testing rather than focusing on just one symptom
- Be willing to discuss various treatment approaches
- Recognize that PCOS management is highly individual
After Diagnosis: First Steps in PCOS Management
If you receive a PCOS diagnosis, these initial strategies can help manage your symptoms:
Nutrition Approaches
- Focusing on blood sugar balance with approaches like a low-carb PCOS diet
- Incorporating low glycemic snacks to maintain energy and reduce cravings
- Understanding how different foods impact blood sugar, which we discuss in articles like the glycemic index of bagels
- Finding the right balance of macronutrients for your specific PCOS type
Lifestyle Modifications
- Regular physical activity that you enjoy, with consideration for whether HIIT workouts are appropriate for your PCOS
- Stress management techniques like meditation, yoga, or breathing exercises
- Optimizing sleep quality and quantity
- Reducing environmental endocrine disruptors in personal care and household products
Supplements and Natural Approaches
- Considering supplements like inositol, N-acetylcysteine, or magnesium (discussed in our magnesium guide)
- Exploring herbs that may support hormone balance
- Working with a healthcare provider to determine appropriate supplements for your specific needs
Medical Treatments
- Discussing medication options like metformin, spironolactone, or hormonal contraceptives based on your primary concerns
- Creating a monitoring plan to track progress and adjust treatment as needed
- Addressing specific symptoms with targeted therapies
Hope for Undiagnosed PCOS: You Are Not Alone
If you suspect you have PCOS but haven't received a diagnosis, remember:
- Your symptoms and experiences are valid
- You deserve thorough evaluation and compassionate care
- Self-advocacy is powerful and necessary in obtaining proper diagnosis
- With the right support, PCOS is manageable
- Connecting with others who understand can provide validation and practical advice
The path to diagnosis may be frustrating, but the relief of understanding what's happening in your body—and having a framework for addressing it—is worth the persistence.
Summary: Breaking the Silence on Undiagnosed PCOS
Undiagnosed PCOS affects millions of women who struggle with unexplained symptoms and health challenges.
By raising awareness about the various ways PCOS can present, advocating for proper testing, and seeking knowledgeable healthcare providers, we can reduce the number of women suffering in silence.
Whether you're just beginning to suspect PCOS or have been managing unexplained symptoms for years, know that clarity is possible.
With the right diagnosis comes the power to make informed choices about your health and well-being—choices that can significantly improve your quality of life and long-term health outlook.
Extra Tip: Create a Symptom Journal
If you suspect you might have undiagnosed PCOS, start tracking your symptoms in a daily journal. Note patterns related to your menstrual cycle, energy levels, mood changes, food reactions, sleep quality, and physical symptoms.
This detailed record can be invaluable when consulting healthcare providers, as it provides concrete data about your experiences over time. Many women find that symptoms they hadn't connected suddenly show clear patterns when tracked consistently, strengthening their case for proper evaluation.
How This Article Was Made
This article was created through a comprehensive review of medical literature on PCOS diagnosis, prevalence of undiagnosed PCOS, and clinical guidelines for evaluation and management. We consulted peer-reviewed studies, epidemiological data, and clinical practice guidelines.
Key sources included:
- Research on PCOS prevalence and diagnosis rates from journals like Fertility and Sterility and the Journal of Clinical Endocrinology & Metabolism
- Clinical practice guidelines from the Endocrine Society and the American Society for Reproductive Medicine
- Epidemiological studies on PCOS across different populations
- Research on diagnostic delays and barriers to PCOS diagnosis
We strive to provide accurate, evidence-based information while acknowledging the real-life experiences of women navigating the complex path to PCOS diagnosis and management.
Community Comments
Community Comments
Add a comment